Respiratory System
Table of Content |
 Respiratory System
Respiratory System
A pair of external nostrils opens out above the upper lips. It leads to a nasal chamber through the nasal passage.
The nasal chamber opens into nasopharynx, which is a portion of pharynx, the common passage for food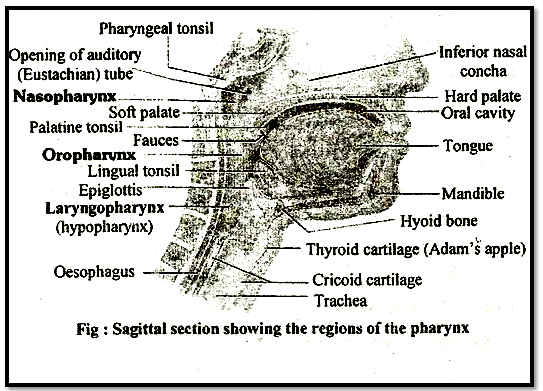
Nasopharynx opens through glottis of the larynx region into the trachea. Larynx is a cartilaginous box which helps in sound production and hence called the sound box.
During swallowing glottis can be covered by a thin elastic cartilaginous flap called epiglottis to prevent the entry of food into the larynx.
Trachea is a straight tube extending up to the mid thoracic cavity, which divides at the level of 5th thoracic vertebra into a right and left primary bronchi. Each bronchi undergoes repeated divisions to form the secondary and tertiary bronchi and bronchioles ending up in very thin terminal bronchioles, The tracheae, primary, secondary and tertiary bronchi, and initial bronchioles are supported by incomplete cartilaginous rings. Each terminal bronchiole gives rise to a number of very thin, irregular walled and vascularised bag like structures called alveoli. The branching network of bronchi, bronchioles and alveoli comprise the lungs.
We have two lungs which are covered by a double layered pleura, with pleural fluid between them. It reduces friction on the lung surface. The outer pleural membrane is in close contact with the thoracic lining whereas the inner pleural membrane is in contact with the lung surface.
The part starting with the external nostrils up to the terminal bronchioles constitute the conducting part whereas the alveoli and their ducts form the respiratory or exchange part of the respiratory system. The conducting part transports the atmospheric air to the alveoli, clears it from foreign particles, humidifies and also brings the air to body temperature. Exchange part is the site of actual diffusion of O2 and CO2 between blood and atmospheric air.
The lungs are situated in the thoracic chamber which is anatomically an air-tight chamber. The thoracic chamber is formed dorsally by the vertebral column, ventrally by the sternum, laterally by the ribs and on the lower side by the dome-shaped diaphragm. The anatomical setup of lungs in thorax is such that any change in the volume of the thoracic cavity will be reflected in the lung (pulmonary) cavity. Such an arrangement is essential for breathing, as we cannot directly alter the pulmonary volume.
Respiration involves the following steps:
(i) Breathing or pulmonary ventilation by which atmospheric air is drawn in and CO2 rich alveolar air is released out.
(ii) Diffusion of gases (O2 and CO2) across alveolar membrane.
(iii) Transport of gases by the blood.
(iv) Diffusion of O2 and CO2 between blood and tissues.
(v) Utilisation of O2 by the cells for catabolic reactions rod resultant release of CO2.
Mechanism of Breathing
Breathing involves two stages: inspiration during which atmospheric air is drawn in and expiration by which the alveolar air is released out.
The movement of air into and out of the lungs is carried out by creating a pressure gradient between the lungs and the atmosphere. Inspiration can occur if the pressure within the lungs (intra-pulmonary pressure) is less than the atmospheric pressure, i.e., there is a negative pressure in the lungs with respect to atmospheric pressure. Similarly; expiration takes place when the intra-pulmonary pressure is higher than the atmospheric pressure. The diaphragm and a specialised set of muscles external and internal intercostals between the ribs, help in generation of such gradients.
Inspiration is initiated by the contraction of diaphragm which increases the volume of thoracic chamber· in the anterod posterior axis. The contraction of external inter-costal muscles lifts up the ribs and the sternum causing an increase in the volume of the thoracic chamber in the dorso-ventral axis. The overall increase in the thoracic volume causes a similar increase in pulmonary volume. An increase in pulmonary volume decreases the intrapulmonary pressure to less than the atmospheric pressure which forces the air from outside to move into the lungs, i.e., inspiration
Relaxation of the diaphragm and the inter-costal muscles returns the diaphragm and sternum to their normal positions and reduce the thoracic volume and thereby the pulmonary volume. This leads to an increase in intra-pulmonary pressure to slightly above the atmospheric pressure causing the expulsion of air from the lungs, i.e., expiration.
On an average, a healthy human breathes 12-16 times/minute.
Respiratory Volumes and Capacities
Tidal Volume (TV): Volume of air inspired or expired during a normal respiration. It is approx. 500 mL., i.e., a healthy man can inspire or expire approximately 6000 to 8000 mL of air per minute.
Inspiratory Reserve Volume (IRV): Additional volume of air, a person can inspire by a forcible inspiration. This averages 2500 mL to 3000 mL.
Expiratory Reserve Volume (ERV): Additional volume of air, a person can expire by a forcible expiration. This averages 1000 mL to 1100 mL.
Residual Volume (RV): Volume of air remaining in the lungs even after a forcible expiration. This averages 1100 mL to 1200 mL. By adding up a few respiratory volumes described above, one can derive various pulmonary capacities, which can be used in clinical diagnosis.
Inspiratory Capacity (IC): Total volume of air a person can inspire after a normal expiration. This includes tidal volume and inspiratory reserve volume (TV + IRV).
Expiratory Capacity (EC): Total volume of air a person can expire after a normal inspiration. This includes tidal volume and expiratory reserve volume (TV+ERV).
Functional Residual Capacity (FRC): Volume of air that will remain in the lungs after a normal expiration. This includes ERV+RV.
Vital Capacity (VC): The maximum volume of air a person can breathe in after a forced expiration. This includes ERV, TV and IRV or the maximum volume of air a person can breathe out after a forced inspiration.
Total Lung Capacity: Total volume of air accommodated in the lungs at the end of a forced inspiration. This includes RV, ERV, TV and IRV or vital capacity + residual volume.
Exchange of Gases
Alveoli are the: primary sites of exchange of gases. Exchange of gases also occur between blood and tissues O2 and CO2 are exchanged in these sites by simple diffusion mainly based on pressure/ concentration gradient. Solubility of the gases as well as the thickness of the membranes involved in diffusion are also some important factors that can affect the rate of diffusion.
A concentration gradient is present for oxygen from alveoli to blood and blood to tissues. Similarly, direction, i.e., from tissues to blood and blood to alveoli. As the solubility of CO2 is 20-25 times higher than that of O2, the amount of CO2 that can diffuse through the diffusion membrane per unit difference in partial pressure is much higher compared to that of O2.
The diffusion membrane is made up of three major layers namely, the thin squamous epithelium of alveoli, the endothelium of alveolar capillaries and the basement substance in between them.
All the factors in our body are favourable for diffusion of O2 from alveoli to tissues and that of CO2 from tissues to alveoli.
Transport of Gases
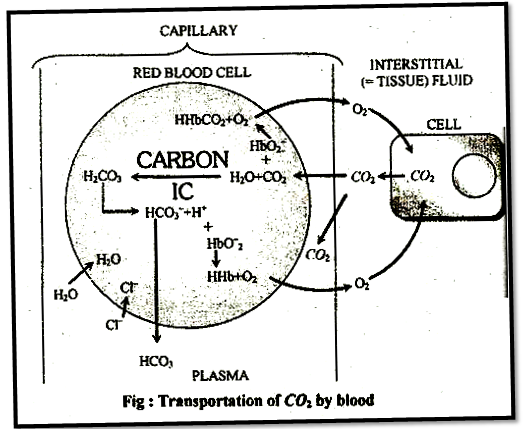
Blood is the medium of transport for O2 and CO2. About 97 per cent of O2 is transported by RBCs in the blood. The remaining 3 per cent of O2 is carried in a dissolved state through the plasma. Nearly 20-25 per cent of CO2 is transported by RBCs whereas 70 per cent of it is carried as bicarbonate. About 7 per cent of CO2 is carried in a dissolved state through plasma.
Transport of Oxygen
Haemoglobin is a red coloured iron containing pigment present in the RBCs. O2 can bind with haemoglobin in a reversible manner to form oxyhaemoglobin.
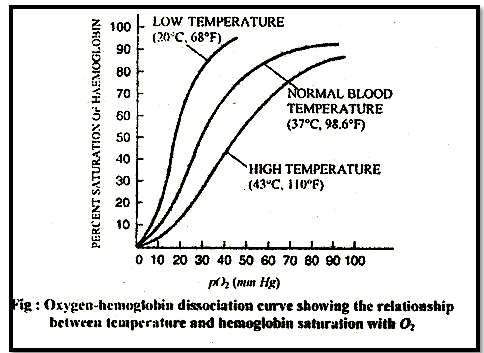
Each haemoglobin molecule can carry a maximum of four molecules of O2. Binding of oxygen with haemoglobin is primarily related to partial pressure of O2. Partial pressure of CO2, hydrogen ion concentration and temperature are the other factors which can interfere with this binding. A sigmoid curve is obtained when percentage saturation of haemoglobin with O2 is plotted against the pO2. This curve is called the Oxygen dissociation curve and is highly useful in studying the effect of factors like pCO2, H+ concentration, etc., on binding of O2 with haemoglobin.
Bohr's effect: Hb-O2 dissociation curve shifts to right when tension in blood is high. Bohr discovered this effect in 1904. Bohr effect is the effect of CO2 on oxyhaemoglobin. Deoxygenation of oxygaernoglobin is directly proportional to blood pCO2. Extent of Bohr's effect depends up on the tension of CO2 in blood only. CO2 of tissue fluid and alveoli does not exert Bohr's effect. During exercise, muscles need mere O2 and want to remove CO2 which has high production. Because of pressure gradient CO2 moves from tissues fluid to capillary blood ® Exert Bohr's effect ® O2 release is hastened from Hb-O2 i.e. Hb-O2 curve shifts to right.In the alveoli, where there is high pO2 gets low pCO2, lesser H+ concentration and lower temperature, the factors are all favourable for the formation of oxvhaemoglobin, whereas in the tissues, where low pO2, high pCO2, high H+ concentration and higher temperature exist, the conditions are favourable for dissociation of oxygen from the oxyhaemoglobin. This clearly indicates that O2 gets bound to haemoglobin in the lung surface. and gets dissociated at the tissues.
Every 100 ml of oxygenated bleed can deliver around 5 ml of O2 to the tissues under normal physiological conditions.
Transport of Carbon Dioxide
CO2 is carried by haemoglobin as carbaminohaemoglobin (about 20-25 per cent). This binding is related to the partial pressure of CO2, pO2 is a major factor which could affect this binding. When pCO2 is high and pO2 is low as in the tissues, mere binding of carbon dioxide occurs whereas, when the pCO2 is low and pO2 is high as in the alveoli, dissociation of CO2 from carbaminohaemoglobin takes place, i.e., CO2 which is bound to haemoglobin from the tissues is delivered at the alveoli.
RBCs contain a very high concentration of the enzyme, carbonic anhydrase and minute quantities of the same is present in the plasma tee. This enzyme facilitates the following reaction in beth directions.
At the tissue site where partial pressure of pCO2 is high due to catabolism, CO2 diffuses into bleed (RBCs and plasma) and forms HCO3 and H+.
At the alveolar site where pCO2 is low, the reaction proceeds in the opposite direction leading to the formation of CO2 and H2O.
CO2 trapped as bicarbonate at the tissue level and transported to the alveoli is released out as CO2.
Every 100 ml of deoxygenated bleed delivers approximately 4 ml of CO2 to the alveoli.
To read more, Buy study materials of Breathing and Exchanges of Gases comprising study notes, revision notes, video lectures, previous year solved questions etc. Also browse for more study materials on Biology here.
View courses by askIITians


Design classes One-on-One in your own way with Top IITians/Medical Professionals
Click Here Know More

Complete Self Study Package designed by Industry Leading Experts
Click Here Know More

Live 1-1 coding classes to unleash the Creator in your Child
Click Here Know More